

Monitoring and Early Warning of Atmospheric Pathogenic Microorganisms: A Review of Recent Studies
Received date: 2025-02-04
Revised date: 2025-04-01
Online published: 2025-03-29
Supported by
the Collaborative Research Project of the National Natural Science Foundation of China and the Chinese Academy of Sciences(L2224041/XK2022DXC005);Self-supporting Program of Guangzhou Laboratory(SRPG22-007);National Funded Postdoctoral Researcher Program(GZC20231001)
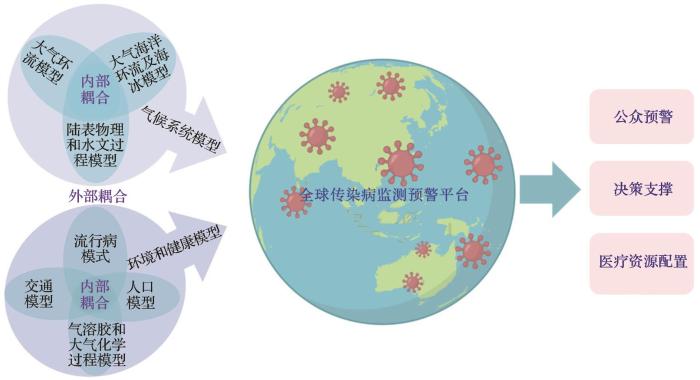
The monitoring and early warning of pathogenic microorganisms and infectious diseases serve as a critical foundation for preventing major public health crises and mitigating biosecurity risks. However, research on the monitoring and early warning of pathogenic microorganism transmission in the atmosphere remains limited, with no systematic framework established yet. This study addresses strategic needs in public health security by identifying key scientific challenges in the field, systematically elucidating the environmental response mechanisms of atmospheric pathogens under climate change, monitoring technologies for pathogenic microorganisms in the atmosphere, and advances in infectious disease prediction models. Furthermore, this study identifies critical research frontiers for future breakthroughs, including: elucidating the source characteristics, formation mechanisms, environmental evolution, and transmission mechanisms of atmospheric pathogens; developing high-precision real-time monitoring technologies for atmospheric pathogens and establishing a biosafety surveillance network; constructing a multi-disciplinary, multi-scale and multi-model coupled prediction and early warning platform for atmospheric pathogen and infectious diseases. This research framework will provide scientific decision-making support for preventing public health emergencies, effectively enhance biosecurity governance capacity, and offer a scientific paradigm for building a global community of health for all.
Jianping HUANG , Xinbo LIAN , Rui WANG , Danfeng WANG , Zhongwei HUANG , Beidou ZHANG , Shujuan HU . Monitoring and Early Warning of Atmospheric Pathogenic Microorganisms: A Review of Recent Studies[J]. Advances in Earth Science, 2025 , 40(4) : 331 -347 . DOI: 10.11867/j.issn.1001-8166.2025.017
| 1 | SESSITSCH A, WAKELIN S, SCHLOTER M, et al. Microbiome interconnectedness throughout environments with major consequences for healthy people and a healthy planet[J]. Microbiology and Molecular Biology Reviews, 2023, 87(3). DOI: 10.1128/mmbr.00212-22 . |
| 2 | HUANG Jianping, ZHANG Beidou, WANG Danfeng, et al. The new direction of interdisciplinary science in the 21st century: climate change and monitoring and early warning of major epidemic situations[J]. Journal of Lanzhou University (Medical Sciences), 2022, 48(11): 1-3. |
| 黄建平, 张北斗, 王丹凤, 等. 21世纪交叉学科的新方向: 气候变化与重大疫情监测预警[J]. 兰州大学学报(医学版), 2022, 48(11): 1-3. | |
| 3 | LIAN X B, HUANG J P, HUANG R J, et al. Impact of city lockdown on the air quality of COVID-19-hit of Wuhan City[J]. Science of the Total Environment, 2020, 742. DOI: 10.1016/j.scitotenv.2020.140556 . |
| 4 | LI Tiantian, DU Yanjun, MO Yang, et al. Human health risk assessment of heat wave based on vulnerability: a review of recent studies[J]. Journal of Environment and Health, 2014, 31(6): 547-550. |
| 李湉湉, 杜艳君, 莫杨, 等. 基于脆弱性的高温热浪人群健康风险评估研究进展[J]. 环境与健康杂志, 2014, 31(6): 547-550. | |
| 5 | KAN Haidong, CHEN Bingheng. Health effects of global climate change[J]. North Environment, 2001, 26(2): 35-36. |
| 阚海东, 陈秉衡. 全球气候变化的健康效应[J]. 北方环境, 2001, 26(2): 35-36. | |
| 6 | WU Xiaoxu, TIAN Huaiyu, ZHOU Sen, et al. Impact of global change on transmission of human infectious diseases[J]. Science China: Earth Sciences, 2013, 43(11): 1 743-1 759. |
| 吴晓旭, 田怀玉, 周森, 等. 全球变化对人类传染病发生与传播的影响[J]. 中国科学: 地球科学, 2013, 43(11): 1 743-1 759. | |
| 7 | HUANG J P, ZHANG L, LIU X Y, et al. Global prediction system for COVID-19 pandemic[J]. Science Bulletin, 2020, 65(22): 1 884-1 887. |
| 8 | LI Z Q, MENG F C, WU B, et al. Reviewing the progress of infectious disease early warning systems and planning for the future[J]. BMC Public Health, 2024, 24(1). DOI: 10.1186/s12889-024-20537-2 . |
| 9 | DANOVARO R, CORINALDESI C, DELL’ANNO A, et al. Marine viruses and global climate change[J]. FEMS Microbiology Reviews, 2011, 35(6): 993-1 034. |
| 10 | HUANG J P, LIU X Y, ZHANG L, et al. The oscillation-outbreaks characteristic of the COVID-19 pandemic[J]. National Science Review, 2021, 8(8). DOI: 10.1093/nsr/nwab100 . |
| 11 | CAVICCHIOLI R, RIPPLE W J, TIMMIS K N, et al. Scientists’ warning to humanity: microorganisms and climate change[J]. Nature Reviews Microbiology, 2019, 17: 569-586. |
| 12 | LAFFERTY K D. The ecology of climate change and infectious diseases[J]. Ecology, 2009, 90(4): 888-900. |
| 13 | BAYOH M N, LINDSAY S W. Effect of temperature on the development of the aquatic stages of Anopheles gambiae sensu stricto (Diptera: Culicidae)[J]. Bulletin of Entomological Research, 2003, 93(5): 375-381. |
| 14 | LIU Y, NING Z, CHEN Y, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals[J]. Nature, 2020, 582(7 813): 557-560. |
| 15 | STADNYTSKYI V, BAX C E, BAX A, et al. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission[J]. Proceedings of the National Academy of Sciences of the United States of America, 2020, 117(22): 11 875-11 877. |
| 16 | XIAO Y Y, HE L M, CHEN Y, et al. The influence of meteorological factors on tuberculosis incidence in Southwest China from 2006 to 2015[J]. Scientific Reports, 2018, 8(1). DOI: 10.1038/s41598-018-28426-6 . |
| 17 | SMITH G S, SCHOENBACH V J, RICHARDSON D B, et al. Particulate air pollution and susceptibility to the development of pulmonary tuberculosis disease in North Carolina: an ecological study[J]. International Journal of Environmental Health Research, 2014, 24(2): 103-112. |
| 18 | YANG X B, DUAN Q H, WANG J J, et al. Seasonal variation of newly notified pulmonary tuberculosis cases from 2004 to 2013 in Wuhan, China[J]. PLoS One, 2014, 9(10). DOI: 10.1371/journal.pone.0108369 . |
| 19 | DENG Bin, ZHOU Zhigang, MA Zesui, et al. The model of back-propagation neural network about the relationship between meterological factors and pulmonary tuberculosis[J]. International Medicine and Health Guidance News, 2008, 14(1): 17-20. |
| 邓斌, 周志刚, 马泽粦, 等. 肺结核病与气象因素关系的BP神经网络模型研究[J]. 国际医药卫生导报, 2008, 14(1): 17-20. | |
| 20 | ZHANG Qiang, YE Dianxiu, YANG Xianwei, et al. Study on high-risk meteorological indexes during SARS epidemic period[J]. China Public Health, 2004, 20(6): 647-648. |
| 张强, 叶殿秀, 杨贤为, 等. SARS流行期高危气象指标的研究[J]. 中国公共卫生, 2004, 20(6): 647-648. | |
| 21 | CHOI K M, CHRISTAKOS G, WILSON M L. El Ni?o effects on influenza mortality risks in the state of California[J]. Public Health, 2006, 120(6): 505-516. |
| 22 | P?HLKER M L, P?HLKER C, KRüGER O O, et al. Respiratory aerosols and droplets in the transmission of infectious diseases[J]. Reviews of Modern Physics, 2023, 95(4). DOI:10.1103/RevModPhys.95.045001 . |
| 23 | DABISCH P, SCHUIT M, HERZOG A, et al. The influence of temperature, humidity, and simulated sunlight on the infectivity of SARS-CoV-2 in aerosols[J]. Aerosol Science and Technology, 2021, 55(2): 142-153. |
| 24 | PAITAL B, AGRAWAL P K. Air pollution by NO2 and PM2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review[J]. Environmental Chemistry Letters, 2021, 19(1): 25-42. |
| 25 | BAYLIS M. Potential impact of climate change on emerging vector-borne and other infections in the UK[J]. Environmental Health, 2017, 16(Suppl. 1). DOI: 10.1186/s12940-017-0326-1 . |
| 26 | REDSHAW C H, STAHL-TIMMINS W M, FLEMING L E, et al. Potential changes in disease patterns and pharmaceutical use in response to climate change[J]. Journal of Toxicology and Environmental Health Part B, Critical Reviews, 2013, 16(5): 285-320. |
| 27 | SEMENZA J C, HERBST S, RECHENBURG A, et al. Climate change impact assessment of food- and waterborne diseases[J]. Critical Reviews in Environmental Science and Technology, 2012, 42(8): 857-890. |
| 28 | PAZ S. Climate change impacts on West Nile virus transmission in a global context[J]. Philosophical Transactions of the Royal Society of London Series B, Biological Sciences, 2015, 370(1 665). DOI: 10.1098/rstb.2013.0561 . |
| 29 | HUIZINGA H W, MCLAUGHLIN G L. Thermal ecology of Naegleria fowleri from a power plant cooling reservoir[J]. Applied and Environmental Microbiology, 1990, 56(7): 2 200-2 205. |
| 30 | EL-SAYED A, KAMEL M. Climatic changes and their role in emergence and re-emergence of diseases[J]. Environmental Science and Pollution Research International, 2020, 27(18): 22 336-22 352. |
| 31 | MOORE S, SHRESTHA S, TOMLINSON K W, et al. Predicting the effect of climate change on African trypanosomiasis: integrating epidemiology with parasite and vector biology[J]. Journal of the Royal Society, Interface, 2012, 9(70): 817-830. |
| 32 | TONG M X, HANSEN A, HANSON-EASEY S, et al. Infectious diseases, urbanization and climate change: challenges in future china[J]. International Journal of Environmental Research and Public Health, 2015, 12(9): 11 025-11 036. |
| 33 | PAYNTER S, WARE R S, WEINSTEIN P, et al. Childhood pneumonia: a neglected, climate-sensitive disease?[J]. Lancet, 2010, 376(9 755): 1 804-1 805. |
| 34 | XU Z W, HU W B, TONG S L. Temperature variability and childhood pneumonia: an ecological study[J]. Environmental Health, 2014, 13(1). DOI: 10.1186/1476-069X-13-51 . |
| 35 | TOWERS S, CHOWELL G, HAMEED R, et al. Climate change and influenza: the likelihood of early and severe influenza seasons following warmer than average winters[J]. PLoS Currents, 2013, 5. DOI: 10.1371/currents.flu.3679b56a3a5313dc7c043fb944c6f138 . |
| 36 | DONALDSON G C. Climate change and the end of the respiratory syncytial virus season[J]. Clinical Infectious Diseases, 2006, 42(5): 677-679. |
| 37 | ZHANG X L, SHAO X J, WANG J, et al. Temporal characteristics of respiratory syncytial virus infection in children and its correlation with climatic factors at a public pediatric hospital in Suzhou[J]. Journal of Clinical Virology, 2013, 58(4): 666-670. |
| 38 | The World Meteorological Organization[Z]. State of the global climate 2024. 2025. |
| 39 | NI J M, ZHAO Y, LI B, et al. Investigation of the impact mechanisms and patterns of meteorological factors on air quality and atmospheric pollutant concentrations during extreme weather events in Zhengzhou City, Henan Province[J]. Atmospheric Pollution Research, 2023, 14(12). DOI:10.1016/j.apr.2023.101932 . |
| 40 | HAMBLETON I R, JEYASEELAN S M, MURPHY M M. COVID-19 in the Caribbean small island developing states: lessons learnt from extreme weather events[J]. The Lancet Global Health, 2020, 8(9): e1114-e1115. |
| 41 | PATZ J A, ENGELBERG D, LAST J. The effects of changing weather on public health[J]. Annual Review of Public Health, 2000, 21: 271-307. |
| 42 | Lemonick D M. Epidemics after natural disasters[J]. American Journal of Medicine, 2011, 8: 144-152. |
| 43 | LIAN X B, HUANG J P, LI H, et al. Cold waves accelerate the spread of infectious diseases[J]. Geophysical Research Letters, 2024, 51(15). DOI: 10.1029/2024GL109405 . |
| 44 | TIAN Huaiyu. 2019-nCoV: new challenges from coronavirus[J]. Chinese Journal of Preventive Medicine, 2020, 54(3):235-238. |
| 田怀玉. 2019-nCoV:来自冠状病毒的新挑战[J]. 中华预防医学杂志, 2020, 54: 4(3):235-238. | |
| 45 | LIAN X B, HUANG J P, LI H, et al. Heat waves accelerate the spread of infectious diseases[J]. Environmental Research, 2023, 231. DOI: 10.1016/j.envres.2023.116090 . |
| 46 | WANG C C, PRATHER K A, SZNITMAN J, et al. Airborne transmission of respiratory viruses[J]. Science, 2021, 373(6 558). DOI: 10.1126/science.abd9149 . |
| 47 | GUO Y M, WU Y, WEN B, et al. Floods in China, COVID-19, and climate change[J]. The Lancet Planetary Health, 2020, 4(10): e443-e444. |
| 48 | WALTON D, van AALST M. Climate-related extreme weather events and COVID-19: a first look at the number of people affected by intersecting disasters[R]. IFRC, Red Cross Red Crescent Climate Centre, 2020. |
| 49 | MORENS D M, FOLKERS G K, FAUCI A S. The challenge of emerging and re-emerging infectious diseases[J]. Nature, 2004, 430(6 996): 242-249. |
| 50 | HARUN N S, LACHAPELLE P, DOUGLASS J. Thunderstorm-triggered asthma: what we know so far[J]. Journal of Asthma and Allergy, 2019, 12: 101-108. |
| 51 | CHANG H Y, LI M J, WANG Y, et al. Acute effects of low temperatures and cold waves on elderly infectious pneumonia mortality-Jinan City, Shandong Province, China, 2014-2022[J]. China CDC Weekly, 2024, 6(5): 77-82. |
| 52 | LIU Z D, ZHANG J, ZHANG Y, et al. Effects and interaction of meteorological factors on influenza: based on the surveillance data in Shaoyang, China[J]. Environmental Research, 2019, 172: 326-332. |
| 53 | SMITH G S, MESSIER K P, CROOKS J L, et al. Extreme precipitation and emergency room visits for influenza in Massachusetts: a case-crossover analysis[J]. Environmental Health, 2017, 16(1). DOI: 10.1186/s12940-017-0312-7 . |
| 54 | MCMICHAEL A J. Extreme weather events and infectious disease outbreaks[J]. Virulence, 2015, 6(6): 543-547. |
| 55 | XING W L, LIU Y Y, WANG H L, et al. A high-throughput, multi-index isothermal amplification platform for rapid detection of 19 types of common respiratory viruses including SARS-CoV-2[J]. Engineering, 2020, 6(10): 1 130-1 140. |
| 56 | LI S L, GUO J Z, GU Y, et al. Assessing airborne transmission risks in COVID-19 hospitals by systematically monitoring SARS-CoV-2 in the air[J]. Microbiology Spectrum, 2023, 11(6). DOI: 10.1128/spectrum.01099-23 . |
| 57 | LI H Q, XU M R, AN X L, et al. High-risk ARGs (HRA) chip: a high-throughput qPCR-based array for assessment of high-risk ARGs from the environment[J]. Water Research, 2024, 262. DOI:10.1016/j.watres.2024.122106 . |
| 58 | LI H, HONG Y W, GAO M K, et al. Distinct responses of airborne abundant and rare microbial communities to atmospheric changes associated with Chinese New Year[J]. iMeta, 2023, 2(4). DOI: 10.1002/imt2.140 . |
| 59 | LI Jing, YAO Maosheng. State-of-the-art status on airborne antibiotic resistant bacteria and antibiotic resistance genes[J]. Chinese Journal of Preventive Medicine, 2018, 52(4): 440-445. |
| 李菁, 要茂盛. 空气介质中耐药细菌和耐药基因的研究进展[J]. 中华预防医学杂志, 2018, 52(4): 440-445. | |
| 60 | CáCERES C J, RAJAO D S, PEREZ D R. Airborne transmission of avian origin H9N2 influenza A viruses in mammals[J]. Viruses, 2021, 13(10). DOI: 10.3390/v13101919 . |
| 61 | SPIEGELMAN D, WHISSELL G, GREER C W. A survey of the methods for the characterization of microbial consortia and communities[J]. Canadian Journal of Microbiology, 2005, 51(5): 355-386. |
| 62 | ARGOTTE-RAMOS R, CIME-CASTILLO J, VARGAS V, et al. Development of an Enzyme-Linked Immunosorbent Assay (ELISA) as a tool to detect NS1 of dengue virus serotype 2 in female Aedes aegypti eggs for the surveillance of dengue fever transmission[J]. Heliyon, 2024, 10(8). DOI: 10.1016/j.heliyon.2024.e29329 . |
| 63 | GREEN M R, SAMBROOK J. Screening colonies by Polymerase Chain Reaction (PCR)[J]. Cold Spring Harbor Protocols, 2019, 2019(6). DOI: 10.1101/pdb.prot095224 . |
| 64 | KUBISTA M, ANDRADE J M, BENGTSSON M, et al. The real-time polymerase chain reaction[J]. Molecular Aspects of Medicine, 2006, 27(2/3): 95-125. |
| 65 | PAV?I? J, ?EL J, MILAVEC M. Assessment of the real-time PCR and different digital PCR platforms for DNA quantification[J]. Analytical and Bioanalytical Chemistry, 2016, 408(1): 107-121. |
| 66 | HUANG Z W, YU X R, LIU Q T, et al. Bioaerosols in the atmosphere: a comprehensive review on detection methods, concentration and influencing factors[J]. Science of the Total Environment, 2024, 912. DOI:10.1016/j.scitotenv.2023.168818 . |
| 67 | WANG L, QI W Z, LIU Y J, et al. Recent advances on bioaerosol collection and detection in microfluidic chips[J]. Analytical Chemistry, 2021, 93(26): 9 013-9 022. |
| 68 | PARK J W, KIM H R, HWANG J. Continuous and real-time bioaerosol monitoring by combined aerosol-to-hydrosol sampling and ATP bioluminescence assay[J]. Analytica Chimica Acta, 2016, 941: 101-107. |
| 69 | CHEN H X, QI X, ZHANG L, et al. COVID-19 screening using breath-borne volatile organic compounds[J]. Journal of Breath Research, 2021, 15(4). DOI: 10.1088/1752-7163/ac2e57 . |
| 70 | WANG Y K, HUANG Z W, ZHOU T, et al. Identification of fluorescent aerosol observed by a spectroscopic lidar over northwest China[J]. Optics Express, 2023, 31(13): 22 157-22 169. |
| 71 | LEE I, SEOK Y, JUNG H, et al. Integrated bioaerosol sampling/monitoring platform: field-deployable and rapid detection of airborne viruses[J]. ACS Sensors, 2020, 5(12): 3 915-3 922. |
| 72 | CHEN E, WAN Dong, CHU Kecheng, et al. The monitoring and research of airborne microbe pollution[J]. Environmental Monitoring in China, 2014, 30(4): 171-178. |
| 陈锷, 万东, 褚可成, 等. 空气微生物污染的监测及研究进展[J]. 中国环境监测, 2014, 30(4): 171-178. | |
| 73 | GUZM?N M, KOURI G, D?AZ M, et al. Dengue, one of the great emerging health challenges of the 21st century[J]. Expert Review of Vaccines, 2004, 3: 511-520. |
| 74 | HUANG Q S, BAKER M, MCARTHUR C, et al. Implementing hospital-based surveillance for severe acute respiratory infections caused by influenza and other respiratory pathogens in new zealand[J]. Western Pacific Surveillance and Response Journal: WPSAR, 2014, 5: 23. |
| 75 | BRAMMER L, BUDD A, COX N. Seasonal and pandemic influenza surveillance considerations for constructing multicomponent systems[J]. Influenza and other respiratory viruses, 2009, 3: 51-58. |
| 76 | LIU Yongqin, GUO Bixi, JI Mukan, et al. A comprehensive dataset of microbial abundance, dissolved organic carbon, and nitrogen in tibetan plateau glaciers[J]. Earth System Science Data, 2022, 14: 2 303-2 314. |
| 77 | YANG Z F, ZENG Z Q, WANG K, et al. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions[J]. Journal of Thoracic Disease, 2020, 12(3): 165-174. |
| 78 | HUANG J P, WANG D F, ZHU Y G, et al. An overview for monitoring and prediction of pathogenic microorganisms in the atmosphere[J]. Fundamental Research, 2024, 4(3): 430-441. |
| 79 | TIAN H Y, LIU Y H, LI Y D, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China[J]. Science, 2020, 368(6 491): 638-642. |
| 80 | BROWNSTEIN J S, RADER B, ASTLEY C M, et al. Advances in artificial intelligence for infectious-disease surveillance[J]. New England Journal of Medicine, 2023, 388(17): 1 597-1 607. |
| 81 | ANDERSON R M, MAY R M. Infectious diseases of humans: dynamics and control[M]. Oxford: Oxford University Press, 1991. |
| 82 | KERMACK W O, MCKENDRICK A G. A contribution to the mathematical theory of epidemics[J]. Proceedings of the Royal Society of London. Series A: Containing Papers of a Mathematical and Physical Character, 1927, 115(772): 700-721. |
| 83 | KERMACK W O, MCKENDRICK A G. Contributions to the mathematical theory of epidemics. II—the problem of endemicity[J]. Proceedings of the Royal Society of London. Series A: Containing Papers of a Mathematical and Physical Character, 1932, 138(834): 55-83. |
| 84 | CASTILLO-CHAVEZ C, CASTILLO-GARSOW CW, A-A YAKUBU. Mathematical models of isolation and quarantine[J]. JAMA, 2003, 290(21): 2 876-2 877. |
| 85 | STEHLé J, VOIRIN N, BARRAT A, et al. Simulation of an SEIR infectious disease model on the dynamic contact network of conference attendees[J]. BMC Medicine, 2011, 9. DOI: 10.1186/1741-7015-9-87 . |
| 86 | OKUWA K, INABA H, KUNIYA T. Mathematical analysis for an age-structured SIRS epidemic model[J]. Mathematical Biosciences and Engineering, 2019, 16(5): 6 071-6 102. |
| 87 | BJ?RNSTAD O N, SHEA K, KRZYWINSKI M, et al. The SEIRS model for infectious disease dynamics[J]. Nature Methods, 2020, 17(6): 557-558. |
| 88 | GRIMM V, MENGEL F, SCHMIDT M. Extensions of the SEIR model for the analysis of tailored social distancing and tracing approaches to cope with COVID-19[J]. Scientific Reports, 2021, 11(1). DOI: 10.1038/s41598-021-83540-2 . |
| 89 | BERGER D W, HERKENHOFF K F, MONGEY S. An seir infectious disease model with testing and conditional quarantine[J]. National Bureau of Economic Research, 2020. DOI:10.2139/ssrn.3561142 . |
| 90 | RǎDULESCU A, WILLIAMS C, CAVANAGH K. Management strategies in a SEIR-type model of COVID 19 community spread[J]. Scientific Reports, 2020, 10(1). DOI: 10.1038/s41598-020-77628-4 . |
| 91 | CARCIONE J M, SANTOS J E, BAGAINI C, et al. A simulation of a COVID-19 epidemic based on a deterministic SEIR model[J]. Frontiers in Public Health, 2020, 8. DOI: 10.3389/fpubh.2020.00230 . |
| 92 | MENDA K, LAIRD L, KOCHENDERFER M J, et al. Explaining COVID-19 outbreaks with reactive SEIRD models[J]. Scientific Reports, 2021, 11(1). DOI: 10.1038/s41598-021-97260-0 . |
| 93 | POONIA R C, SAUDAGAR A K J, ALTAMEEM A, et al. An enhanced SEIR model for prediction of COVID-19 with vaccination effect[J]. Life, 2022, 12(5). DOI: 10.3390/life12050647 . |
| 94 | KISELEV I N, AKBERDIN I R, KOLPAKOV F A. Delay-differential SEIR modeling for improved modelling of infection dynamics[J]. Scientific Reports, 2023, 13(1). DOI: 10.1038/s41598-023-40008-9 . |
| 95 | LU M, ZHENG X Y, JIA W N, et al. Analysis and prediction of improved SEIR transmission dynamics model: taking the second outbreak of COVID-19 in Italy as an example[J]. Frontiers in Public Health, 2023, 11. DOI: 10.3389/fpubh.2023.1223039 . |
| 96 | CHEN T M, RUI J, WANG Q P, et al. A mathematical model for simulating the phase-based transmissibility of a novel coronavirus[J]. Infectious Diseases of Poverty, 2020, 9(1). DOI: 10.1186/s40249-020-00640-3 . |
| 97 | LIANG J Y, WANG Y, LIN Z J, et al. Influenza and COVID-19 co-infection and vaccine effectiveness against severe cases: a mathematical modeling study[J]. Frontiers in Cellular and Infection Microbiology, 2024, 14. DOI: 10.3389/fcimb.2024.1347710 . |
| 98 | LI H, HUANG J P, LIAN X B, et al. Impact of human mobility on the epidemic spread during holidays[J]. Infectious Disease Modelling, 2023, 8(4): 1 108-1 116. |
| 99 | DU Zhicheng, HAO Yuancheng, WEI Yongyue, et al. Using Markov Chain Monte Carlo methods to estimate the age-specific case fatality rate of COVID-19[J]. Chinese Journal of Epidemiology, 2020, 41(11): 1 777-1 781. |
| 杜志成, 郝元涛, 魏永越, 等. 基于马尔科夫链蒙特卡罗模拟方法的COVID-19年龄别病死率估计[J]. 中华流行病学杂志, 2020, 41(11): 1 777-1 781. | |
| 100 | KIM J, AHN I. Infectious disease outbreak prediction using media articles with machine learning models[J]. Scientific Reports, 2021, 11(1). DOI: 10.1038/s41598-021-83926-2 . |
| 101 | ZHANG Y M, CHEN K, WENG Y, et al. An intelligent early warning system of analyzing Twitter data using machine learning on COVID-19 surveillance in the US[J]. Expert Systems with Applications, 2022, 198. DOI: 10.1016/j.eswa.2022.116882 . |
| 102 | SU X Y, SUN Y F, LIU H X, et al. An innovative ensemble model based on deep learning for predicting COVID-19 infection[J]. Scientific Reports, 2023, 13. DOI: 10.1038/s41598-023-39408-8 . |
| 103 | HUANG J P, ZHANG L, CHEN B, et al. Development of the second version of global prediction system for epidemiological pandemic[J]. Fundamental Research, 2024, 4(3): 516-526. |
| 104 | XU T, CHENG J, YANG Z F, et al. COVID-19 focused series: diagnosis and forecast of COVID-19[J]. Journal of Thoracic Disease, 2023, 15(3): 1 503-1 505. |
| 105 | YANG L Y, WANG Z M, WANG L, et al. Association of vaccination, international travel, public health and social measures with lineage dynamics of SARS-CoV-2[J]. Proceedings of the National Academy of Sciences of the United States of America, 2023, 120(33). DOI: 10.1073/pnas.2305403120 . |
/
| 〈 |
|
〉 |